A technology initiative launched at CERN to address the lack of radiotherapy in low- and middle-income countries is preparing for its first linear-accelerator prototype, write Deepa Angal-Kalinin, Graeme Burt and Manjit Dosanjh

By 2040, the annual global incidence of cancer is expected to rise by more than 42% from 19.3 million to 27.5 million cases, corresponding to approximately 16.3 million deaths. Shockingly, some 70% of these new cases will be in low- and middle-income countries (LMICs), which lack the healthcare programmes required to effectively manage their cancer burden. While it is estimated that about half of all cancer patients would benefit from radiotherapy (RT) for treatment, there is a significant shortage of RT machines outside high-income countries.
More than 10,000 electron linear accelerators (linacs) are currently used worldwide to treat patients with cancer. But only 10% of patients in low-income and 40% in middle-income countries who need RT have access to it. Patients face long waiting times, are forced to travel to neighbouring regions or face insurmountable expenditure to access treatment. In Africa alone, 27 out of 55 countries have no linac-based RT facilities. In those that do, the ratio of the number of machines to people ranges from one machine to 423,000 people in Mauritius, one machine to almost five million people in Kenya and one machine to more than 100 million people in Ethiopia (see “Out of balance” image). In high-income countries such as the US, Switzerland, Canada and the UK, by contrast, the ratio is one RT machine to 85,000, 102,000, 127,000 and 187,000 people, respectively. To draw another stark comparison, Africa has approximately 380 linacs for a population of 1.2 billion while the US has almost 4000 linacs for a population of 331 million.
Unique challenges
It is estimated that to meet the demand for RT in LMICs over the next two to three decades, the current projected need of 5000 RT machines is likely to become more than 12,000. To put these figures into perspective, Varian, the market leader in RT machines, has a current worldwide installation base of 8496 linacs. While many LMICs provide RT using cobalt-60 machines, linacs offer better dose-delivery parameters and better treatment without the environmental and potential terrorism risks associated with cobalt-60 sources. However, since linacs are more complex and labour-intensive to operate and maintain, their current costs are significantly higher than cobalt-60 machines, both in terms of initial capital costs and annual service contracts. These differences pose unique challenges in LMICs, where macro- and micro-economic conditions can influence the ability of these countries to provide linac-based RT.
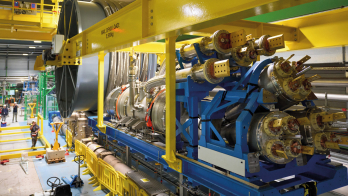
In November 2016 CERN hosted a first-of-its-kind workshop, sponsored by the International Cancer Expert Corps (ICEC), to discuss the design characteristics of RT linacs (see “Linac essentials” image) for the challenging environments of LMICs. Leading experts were invited from international organisations, government agencies, research institutes, universities and hospitals, and companies that produce equipment for conventional X-ray and particle therapy. The following October, CERN hosted a second workshop titled “Innovative, robust and affordable medical linear accelerators for challenging environments”, co-sponsored by the ICEC and the UK’s Science and Technology Facilities Council, STFC. Additional workshops have taken place in March 2018, hosted by STFC in collaboration with CERN and the ICEC, and in March 2019, hosted by STFC in Gaborone, Botswana (see “Healthy vision” image). These and other efforts have identified substantial opportunities for scientific and technical advancements in the design of the linac and the overall RT system for use in LMICs. In 2019, the ICEC, CERN, STFC and Lancaster University entered into a formal collaboration agreement to continue concerted efforts to develop this RT system.
The idea of novel medical linacs is an excellent example of the impact of fundamental research on wider society
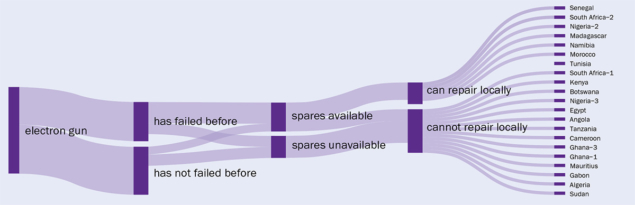
In June 2020, STFC funded a project called ITAR (Innovative Technologies towards building Affordable and equitable global Radiotherapy capacity) in partnership with the ICEC, CERN, Lancaster University, the University of Oxford and Swansea University. ITAR’s first phase was aimed at defining the persistent shortfalls in basic infrastructure, equipment and specialist workforce that remain barriers to effective RT delivery in LMICs. Clearly, a linac suitable for these conditions needs to be low-cost, robust and easy to maintain. Before specifying a detailed design, however, it was first essential to assess the challenges and difficulties RT facilities face in LMICs and in other demanding environments. Published in June 2021, an expansive study of RT facilities in 28 African countries was carried out and compared to western hospitals by the ITAR team to quantitatively and qualitatively assess and compare variables in several domains (see “Downtime” figure). The survey builds on a related 2018 study on the availability of RT services and barriers to providing such services in Botswana and Nigeria, which looked at the equipment maintenance logs of linacs in those countries and selected facilities in the UK.
Surveying the field
The absence of detailed data regarding linac downtime and failure modes makes it difficult to determine the exact impact of the LMIC environment on the performance of current technology. The ongoing ITAR design development and prototyping process identified a need for more information on equipment failures, maintenance and service shortcomings, personnel, training and country-specific healthcare challenges from a much larger representation of LMICs. A further-reaching ITAR survey obtained relevant information for defining design parameters and technological choices based on issues raised at the workshops. They include well-recognised factors such as ease and reliability of operation, machine self-diagnostics and a prominent display of impending or actual faults, ease of maintenance and repair, insensitivity to power interruptions, low power requirement and the consequent reduced heat production.

Based on the information from its surveys, ITAR produced a detailed specification and conceptual design for an RT linac that requires less maintenance, has fewer failures and offers fast repair. Over the next three years, under the umbrella of a larger project called STELLA (Smart Technologies to Extend Lives with Linear Accelerators) launched in June 2020, the project will progress to a prototype development phase at STFC’s Daresbury Laboratory.
The design of the electron gun has been optimised to increase beam-capture. This has the dual advantage of reducing both the peak current required from the gun to deliver the requisite dose and “back bombardment”. It also allows for simpler replacement of the electron gun’s cathode by trained personnel (current designs require replacement of the full electron gun or even the full linac). Electron-beam capture is limited in medical linacs as the pulses from the electron gun are much longer in duration than the radiofrequency (RF) period, meaning electrons are injected at all RF phases. Some phases cause the bunch to be accelerated while others result in electrons being reflected back to the cathode. In typical linacs, less than 50% of electrons reach the target and many electrons reach the target with lower energies. In high-energy accelerators velocity bunching can be used to compress the bunch, however the space is limited in medical linacs and the energy gain per cell is often well in excess of the beam energy. To allow velocity bunching in a medical linac, the first cell needs to operate at a low gradient – such that less space is required to bunch as the average beam velocity is much lower and the deceleration is less than the beam energy. By adjusting the length of the first and second cells, the decelerated electrons can re-accelerate on the next RF cycle and synchronise with the accelerated electrons, capturing nearly all the electrons and transporting them to the target without a low-energy tail. This is achieved using techniques originally developed for the optimisation of klystrons as part of the Compact Linear Collider project at CERN. By adjusting cell-to-cell coupling, it is possible to make all the other cells at a higher gradient similar to a standard medical linac such that the total linac length remains the same (see “Strong coupling” figure).

The electrical power supply in LMICs can often be variable and protection equipment to isolate harmonics between pieces of equipment is not always installed, hence it is critical to consider this when designing the electrical system for RT machines. This in itself is relatively straightforward but is not normally considered as part of a RT machine design.
The failure of multi-leaf collimators (MLCs), which alter the intensity of the radiation so that it conforms to the tumour volume via several individually actuated leaves, is a major linac downtime issue. Designing MLCs that are less prone to failure will play a key role in RT in LMICs, with studies ongoing into ways to simplify the design without compromising on treatment quality.
Building a workforce
Making it simpler to diagnose and repair faults on linacs is another key area that needs improvement. Given the limited technical staff training in some LMICs, when a machine fails it can be challenging for local staff to make repairs. In addition, components that are degrading can be missed by staff, leading to loss of valuable time to order spares. An important component of the STELLA project, led by ICEC, is to enhance existing and establish new twinning programmes that provide mentoring and training to healthcare professionals in LMICs to build workforce capacity and capability in those regions.

The idea to address the need for a novel medical linac for challenging environments was first presented by Norman Coleman, senior scientific advisor to the ICEC, at the 2014 ICTR-PHE meeting in Geneva. This led to the creation of the STELLA project, led by Coleman and ICEC colleagues Nina Wendling and David Pistenmaa, which is now using technology originally developed for high-energy physics to bring this idea closer to reality – an excellent example of the impact of fundamental research on wider society.
The next steps are to construct a full linac prototype to verify the higher capture, as well as to improve the ease of maintaining and repairing the machine. Then we need to have the RT machine manufactured for use in LMICs, which will require many practical and commercial challenges to be overcome. The aim of project STELLA to make RT truly accessible to all cancer patients brings to mind a quote from the famous Nigerian novelist Chinua Achebe: “While we do our good works let us not forget that the real solution lies in a world in which charity will have become unnecessary.”
Further reading
International Atomic Energy Agency: Directory of Radiotherapy Centres (dirac.iaea.org)
T A Ige et al. 2021 Clin. Oncol. 33 e521.